[ad_1]
In today’s competitive market, businesses must prioritize customer retention to ensure long-term success. Engaged customers not only promote brand loyalty but also act as advocates and influencers for the company. Retaining customers is often more cost-effective than acquiring new ones, making it essential to invest in effective strategies. This article explores various tactics to elevate engagement, boost customer satisfaction, and, ultimately, enhance customer retention.
Understanding Customer Engagement
Customer engagement refers to the emotional connection between a business and its customers. It involves the interactions customers have with a brand across multiple channels and touchpoints. A deeper understanding of customer needs, preferences, and behaviors is crucial for crafting engaging experiences that foster long-lasting relationships.
Strategies for Enhancing Customer Retention
1. Personalization
Today’s consumers expect personalized experiences. Leveraging data analytics enables businesses to understand individual customer preferences and tailor offerings accordingly. Personalization can take various forms, including:
- Customized email marketing messages
- Product recommendations based on past purchases
- Targeted promotions and discounts
2. Excellent Customer Service
Your customer service can make or break a customer’s experience with your brand. Offering timely, helpful, and friendly service can significantly boost customer satisfaction and retention. Here are a few pointers on enhancing customer service:
- Train staff to be attentive and responsive to customer needs.
- Utilize chatbots for instant responses to inquiries.
- Encourage customer feedback and act on it promptly.
3. Loyalty Programs
Loyalty programs are effective tools for incentivizing repeat purchases and fostering brand loyalty. By rewarding customers for their loyalty, businesses can keep them coming back. Consider these approaches:
- Points-based systems that offer redeemable rewards.
- Exclusive membership benefits, such as discounts or free products.
- Referral bonuses for recommending new customers.
4. Content Marketing
Providing valuable and relevant content can help establish your brand as a trusted authority in your industry. Engaging blog posts, informative videos, and useful guides can keep customers interested and encourage them to return to your website. Content marketing strategies include:
- Regularly updating the blog with industry trends and tips.
- Creating engaging video tutorials or webinars.
- Utilizing social media to share content and interact with followers.
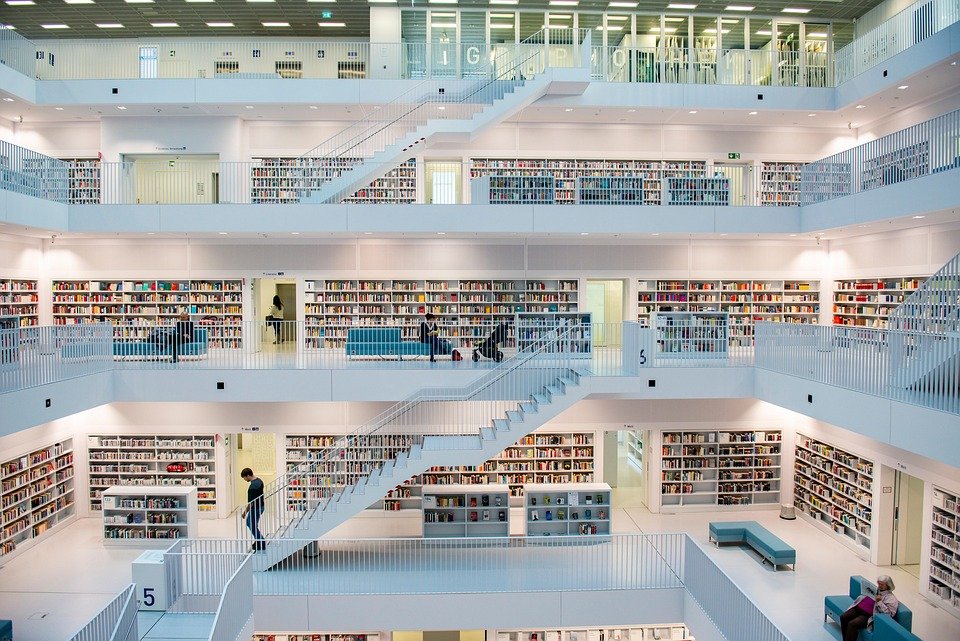
5. Community Building
Creating a sense of belonging can significantly enhance customer loyalty. By building a community around your brand, customers feel valued and more likely to continue their engagement. Consider these methods:
- Creating user forums or social media groups.
- Organizing events or webinars for customers.
- Encouraging user-generated content and testimonials.
6. Customer Feedback and Adaptation
Regularly seeking customer feedback and being open to making changes based on that feedback is vital for retaining engagement. This approach shows customers that their opinions matter and encourages them to stay loyal. Strategies include:
- Conducting surveys after purchase.
- Monitoring reviews and social media mentions.
- Implementing changes based on customer suggestions.
7. Transparent Communication
Transparency builds trust. By maintaining open lines of communication regarding product updates, company news, or potential issues, businesses can strengthen their relationship with customers. Key practices include:
- Regularly updating customers about new products or services.
- Communicating any issues that may affect service quality.
- Being clear about pricing and terms of service.
Conclusion
In a world where options are plentiful, maintaining customer engagement is essential to ensuring loyalty and long-term success. By implementing these strategies—personalization, exceptional customer service, loyalty programs, content marketing, community building, feedback mechanisms, and transparent communication—businesses can foster deeper connections with their customers. Elevating engagement not only improves customer retention but also creates brand advocates who can drive new business through positive word-of-mouth.
FAQs
1. Why is customer retention important?
Customer retention is crucial because acquiring new customers is often more expensive than retaining existing ones. Loyal customers are more likely to make repeat purchases and recommend your brand to others.
2. What is the difference between customer engagement and customer satisfaction?
Customer engagement focuses on the emotional connection and interactions with a brand, while customer satisfaction measures how well a product or service meets customer expectations.
3. How can technology help improve customer retention?
Technology can facilitate personalized communication, automate customer service through chatbots, analyze customer data for insights, and streamline loyalty program management.
4. What role does social media play in customer engagement?
Social media allows businesses to interact directly with customers, share relevant content, gather feedback, and create a sense of community, all of which enhance engagement and retention.
[ad_2]








Leave a Reply